The treatment for liver cancer depends on factors like the size and location of the tumour, your overall health, and whether the cancer has spread. You might need one or more of these treatments:
Alternative 1 – Surgery:
This could mean either removing part of the liver (partial hepatectomy) or replacing the liver with a healthy one from a donor (liver transplant). Not everyone will be able to have surgery.
Alternative 2 – Ablation:
A minimally invasive procedure where a thin wand is inserted through the skin to destroy the tumour using heat or freezing. This works best for small tumours and may cure the cancer.
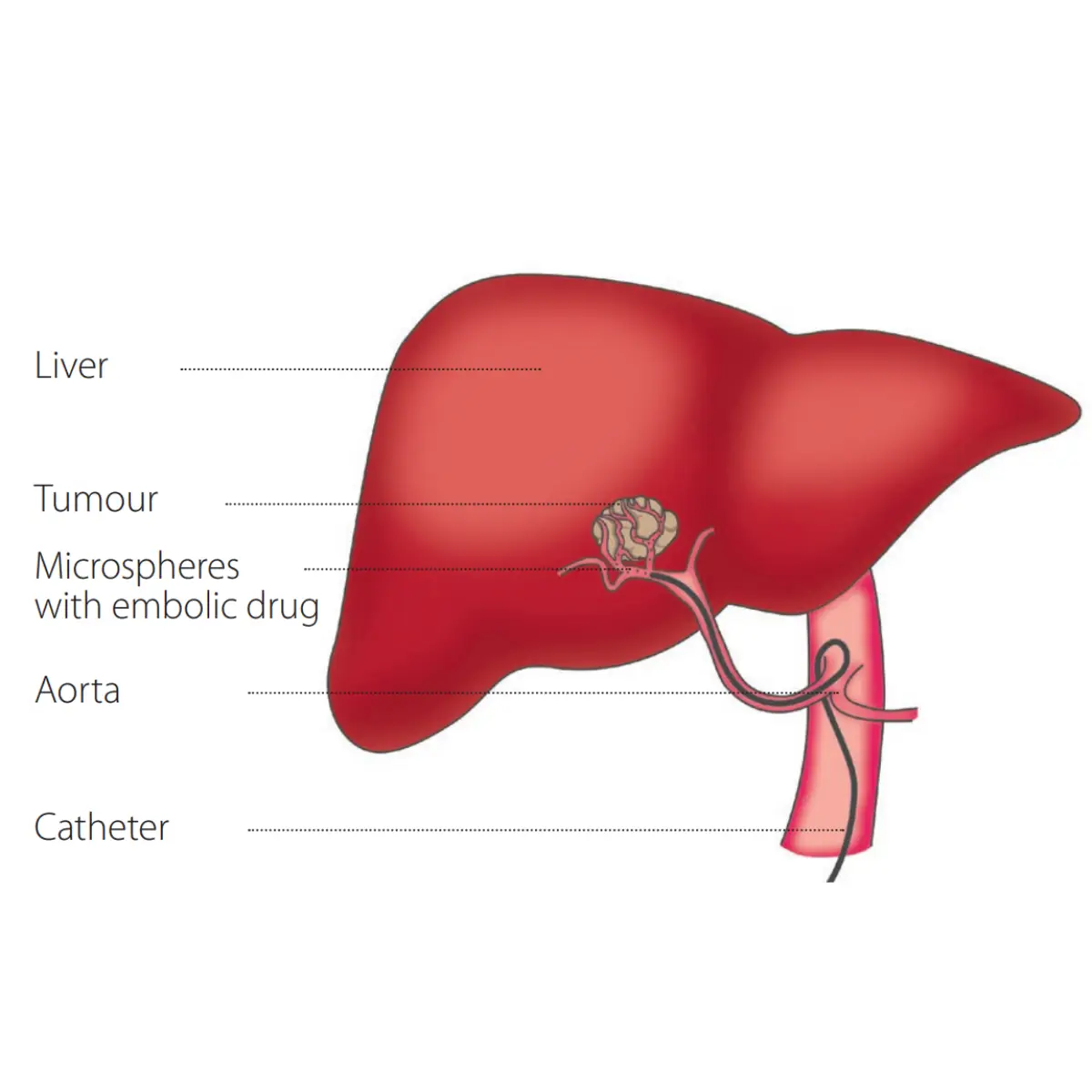
Alternative 3 – Transarterial Radioembolization (TARE):
A minimally invasive procedure that delivers tiny radioactive beads directly into the tumour’s blood supply to shrink it.
Alternative 4 – Radiation Therapy:
External Beam Radiation Therapy (EBRT): a series of treatments that use radiation beams from outside the body to destroy the tumour.
Interventional oncology treatments use imaging techniques (like ultrasound and CT scans) to target the areas causing pain, such as the nerves or tumours. These treatments can include:
🔹 Nerve blocks and injections
🔹 Neurolysis, which works by destroying the nerves causing the pain
🔹 A (percutaneous) ablation uses heat or cold to treat painful tumours
🔹 Augmentation procedures for the bones and the spine